Most people think of diabetes management as a checklist: monitor blood sugar, take insulin, and watch your diet. But did you know that your mouth and your metabolism are constantly talking to each other?
It is a surprising medical fact: Gum disease and diabetes are “bad teammates.”
This relationship is bidirectional, meaning diabetes affects your gums, and surprisingly, untreated gum disease can make your diabetes significantly harder to manage. Understanding this connection is vital for protecting both your smile and your overall health.
At Dr. Gowd’s Dental Hospitals, we believe in treating the whole patient, not just the teeth. Let’s break down this complex relationship in a simple, science-backed way.
1. What Is Gum Disease (Periodontal Disease)?
Before understanding the link, we must understand the infection. Gum disease is a chronic bacterial infection of the gums and the bone supporting your teeth. It is caused mainly by dental plaque—a sticky film of bacteria.
It typically progresses in two distinct stages:
- Gingivitis: The early warning stage. Gums are red, swollen, and bleed easily during brushing. The good news? It is fully reversible with professional cleaning and better hygiene.
- Periodontitis: The advanced stage. The infection spreads deeper, destroying the bone and tissue holding your teeth in place. This leads to gum recession, loose teeth, and eventually tooth loss.
The “Silent” Threat: Gum disease is often painless until it reaches an advanced stage. You might not feel the damage happening until it is too late.
2. The Connection: A Two-Way Street

Research has firmly established that diabetes and gum disease feed off each other.
Part A: How Diabetes Increases the Risk of Gum Disease
People with diabetes (especially uncontrolled diabetes) are up to 3 times more likely to develop severe gum disease. Why?
- Sugar Feeds Bacteria: High glucose levels in your blood also mean higher glucose levels in your saliva. Harmful oral bacteria thrive on this sugar, multiplying faster and forming plaque more aggressively.
- Weakened Immunity: Diabetes weakens the body’s white blood cells, which are your main defense against infections. This makes your gums “lazy” at fighting off the bacteria that cause gingivitis.
- Vascular Damage: Diabetes thickens blood vessels, slowing the flow of nutrients to body tissues and removing harmful wastes. This impairs the gum’s ability to heal.
Part B: How Gum Disease Makes Diabetes Worse
Here is the part most patients don’t know: A dirty mouth can ruin your blood sugar control.
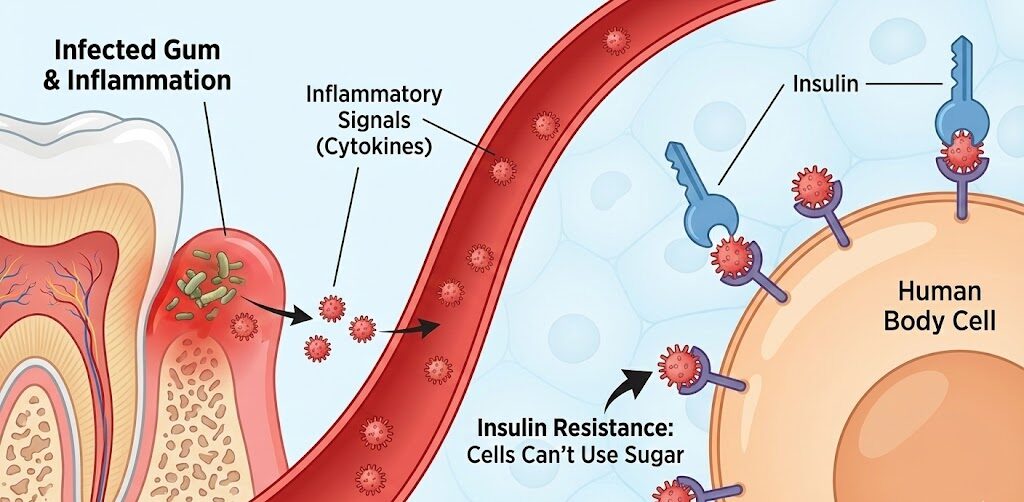
- The Inflammation Factor: Periodontal disease causes low-grade, chronic inflammation throughout the body.
- Insulin Resistance: This inflammation releases chemical signals (cytokines) into the bloodstream. These chemicals block insulin from working effectively.
- The Result: Your body becomes more resistant to insulin, causing blood sugar levels to spike and remain high.
In Short: Inflamed gums = Poor sugar control. Research suggests that untreated periodontal disease can raise HbA1c levels, acting almost like a “sugar spike” that won’t go away.
3. The Vicious Cycle
If left untreated, these two conditions fuel a dangerous cycle:
- Diabetes weakens immunity → Causing Gum Disease.
- Gum Disease increases inflammation → Worsening Insulin Resistance.
- Blood sugar rises → Feeding more gum bacteria.
- The cycle repeats.
The Solution? Break the cycle. You cannot effectively treat one without managing the other.
4. Can Treating Gum Disease Improve Diabetes?
Yes—science says so! Treating gum disease isn’t just about saving teeth; it’s about stabilising your health. Multiple clinical studies have shown that professional periodontal therapies—like Scaling and Root Planing (deep cleaning)—can lead to better blood sugar control.
The Impact: Effective gum disease treatment in Hyderabad can reduce HbA1c levels by 0.4% to 0.6%. While that sounds small, clinically, it is roughly equal to the effect of adding a second diabetes medication!
5. Warning Signs Diabetic Patients Should Never Ignore
If you have diabetes, you must be hyper-aware of these “Red Flags” in your mouth:
- Bleeding Gums: Seeing pink in the sink when you brush is not normal.
- Persistent Bad Breath: Halitosis that doesn’t go away with mouthwash (often caused by bacteria).
- Receding Gums: Your teeth looking “longer” than before.
- Loose Teeth: Or a change in the way your teeth fit together when you bite.
- Dry Mouth: Diabetic patients often suffer from low saliva flow, which increases cavity risk.
6. How to Protect Your Gums (and Your Blood Sugar)
The key to management is a combination of home care and professional help.
- Strict Oral Hygiene: Brush twice daily with a soft-bristle brush and floss every single day.
- Control Blood Sugar: Keep your glucose levels within the target range advised by your physician.
- Hydrate: Drink plenty of water to combat dry mouth.
- Regular Dental Visits: Diabetic patients need more frequent cleanings—typically every 3 to 4 months rather than just once a year.
Looking for expert care? If you are experiencing symptoms and need gum disease treatment in Hyderabad, early intervention is key to preventing irreversible damage.
Frequently Asked Questions (FAQs)
Gingivitis (the early stage) is completely reversible with professional cleaning and good hygiene. However, Periodontitis (advanced gum disease) involves bone loss, which is usually permanent. The goal of treatment is to arrest (stop) the disease from progressing further.
Modern gum disease treatment in Hyderabad at Dr. Gowd’s Dental is comfortable and minimally invasive. We use local anesthesia and advanced laser technology to ensure deep cleanings are performed with little to no discomfort.
Standard patients visit every 6 months, but we recommend that diabetic patients visit every 3 to 4 months. Because diabetic patients heal slower and are more prone to infection, frequent monitoring ensures we catch issues before they become serious.
Most dental insurance plans cover periodontal treatments like scaling and root planing, as they are considered medically necessary, not cosmetic. We recommend checking with your specific provider.
Yes! However, your blood sugar must be well-controlled before the surgery to ensure proper healing and osseointegration (bone fusing to the implant). Uncontrolled diabetes increases the risk of implant failure.
Conclusion: Your Mouth Is Not Separate From Your Body
Gum disease and diabetes are deeply connected. A healthy smile helps control blood sugar, and controlled diabetes helps prevent gum disease. It is about total health, not just teeth.
At Dr. Gowd’s Dental Hospitals, we specialize in managing the oral health of medically compromised patients. Our team understands the delicate balance between diabetes and dentistry.
Don’t let the silent disease affect your life. Contact us today at 8886664790 | www.drgowddental.com
Branches: Banjara Hills | Secunderabad | Hitech Cityto schedule a comprehensive periodontal evaluation.

